Vertebral Compression Fractures
Vertebral Compression Fractures
Vertebral Compression Fractures (VCFs) also known as spinal fractures can occur anywhere in the spine although most commonly they present in the mid (thoracic) and low back (lumbar) regions. They can occur from a number of reasons most commonly after some type of trauma or fall but can happen from cancer that has spread into the spine. They become more common as you get older and are usually associated with osteoporosis/osteopenia, a weakening of your bones that makes them more prone to fractures. Over 40 million Americans are at an increased risk of developing VCFs which is more common in women than men.
In people with severe osteoporosis, a VCF can occur after a simple sneeze or even turning in bed. If there is no history of osteoporosis or if you are in the early stages of osteoporosis, it typically takes more force to cause your spine to fracture such as a fall or a car accident.
How does this occur?
Your spine is made up of bony building blocks called vertebral bodies. These vertebrae sit on top of one another and serve to protect the spinal cord. As you age, these bones become more susceptible to fracturing as the bones weaken and can eventually collapse upon itself. This can cause a significant amount of pain and structurally can cause your posture to stoop forward (kyphosis) and chronically can give you the appearance of a hunchback. Both these factors can leave you bedridden and make it difficult for you to take a deep breath making you more susceptible to infections such as pneumonia.
What do you feel?
Acutely, the main clinical symptom of VCFs is the sudden onset of back pain. This can occur with even little to no trauma. Typically, the pain is worse with standing, walking, bending or twisting and improved with rest or lying on your back. Pressing directly over the area in your back can increase your pain as well.
In addition, pieces of the fracture or even the fracture itself can put pressure on the spinal cord. This can irritate the nerves in your back causing you to experience pain, numbness, tingling and/or weakness around your rib cage, down your arm and down your leg.
What can happen?
Over time, you can become shorter with more limited motion of your spine with the development of a dowager’s hump (hunchback) and a stomach that protrudes (ie sticks out) which can decrease your appetite. Pain can decrease your activity level which leads to more bone loss which further increases your risk of fractures. Not treating fractures can lead to increased risk of more disease and even death.
How do we know you have a fracture?
The majority of time, your history and physical exam will determine if we clinically suspect you of having a fracture. To confirm this, you will likely need to undergo one or more of the following tests:
- X-ray: This is the baseline study you will need to see if you have fracture. Unfortunately, it does not tell us whether your fracture is old or new. In addition, it may be difficult to see small fractures.
- Magnetic resonance imaging (MRI): A diagnostic test that can determine whether you have a fracture or not, if it is old or new and if it impinges or gets close to the spinal cord.
- Computed tomography scan (CT or CAT scan): A diagnostic test that is typically only used if you cannot undergo an MRI. It is excellent at showing the bony architecture but does not do as good a job as the MRI in seeing soft tissue structures such as nerves.
- Bone scan: It is a test used to locate sources of bone inflammation which is present during the early stages of a vertebral compression fracture.
- Dual-energy x-ray absorptiometry (DXA or DEXA) or bone densitometry: This test is used to measure bone density and if osteoporosis exists. This is essentially a low exposure x-ray that detects small changes in bone mass.
How do we treat it?
Traditionally, people who presented with VCFs have been treated with bed rest, medications such as opioids and bracing. Limiting your activity level can lessen the pain but on the other hand can lead to the body becoming deconditioned and possibly even more prone to infections. Pain medications have multiple side effects which include nausea, vomiting and constipation all of which can be worse than the fracture pain itself. Back bracing provides support for the injured spine immobilizing the area until the fracture heals which can take as long as three months. All in all, these treatments may fail to relieve the pain, do not provide long-term functional improvement, may exacerbate bone loss and do not attempt to restore the anatomy.
If there are any neurological deficits, open surgical treatment may be necessary. This typically involves fusing your spine with hardware. Obviously, this can be very invasive and outcomes can be poor when the bone is weak from osteoporosis.
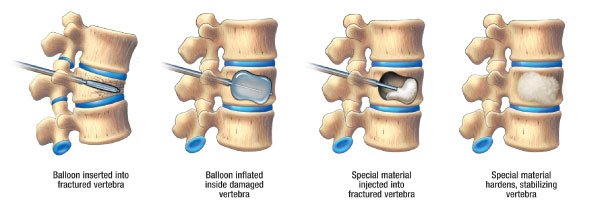
Realizing the importance of treating fractures aggressively to help reduce the pain and the possibility of continued spinal deformity, minimally invasive techniques such vertebroplasty and kyphoplasty were developed. These techniques help to stabilize the fracture by placing cement in the fracture itself. This can provide immediate relief to the pain.
Overall, prevention is the key. To help reduce your chances of having a VCF, you may need to modify your diet and consider resistance training such as swimming. There are also medications available that can decrease the rate of bone loss. Here at VIPSC, we will determine the best way to not only diagnose but treat your fracture while at the same time, develop a treatment plan that will help prevent the development of future fractures.
Get help and advice from Virginia Interventional Pain and Spine Center today
Book a consultation Go back to ConditionsHey there, this is a cookies enabled notification. Close it once and it's closed forever.
Read About Cookies Dismiss